A few years ago, I tore my meniscus. I didn’t realize it at the time, but it was the beginning of my own personal journey with mental health and chronic disease.
Surgery helped temporarily, but my knee has gradually deteriorated over the last few years, slowly turning arthritic. Cortisone shots and other therapies helped temporarily, but lately I’ve been in constant agony—regardless of medication, crutches, or resting.
And as the Pittsburgh winter approaches, my knee is throbbing.
As a therapist, this journey is a powerful reminder: mental health and chronic pain are difficult pathways to navigate.
If you’re dealing with your own chronic illness, your mental health is just as important as your physical health.
Find help in the table of contents, or continue reading to learn more.
Table of Contents
Statistics On Mental Health & Chronic Illness
Complications With Chronic Disease & Mental Illness
Mental Health Therapy For Chronic Disease
Pittsburgh Mental Therapy for Chronic Pain & Illness
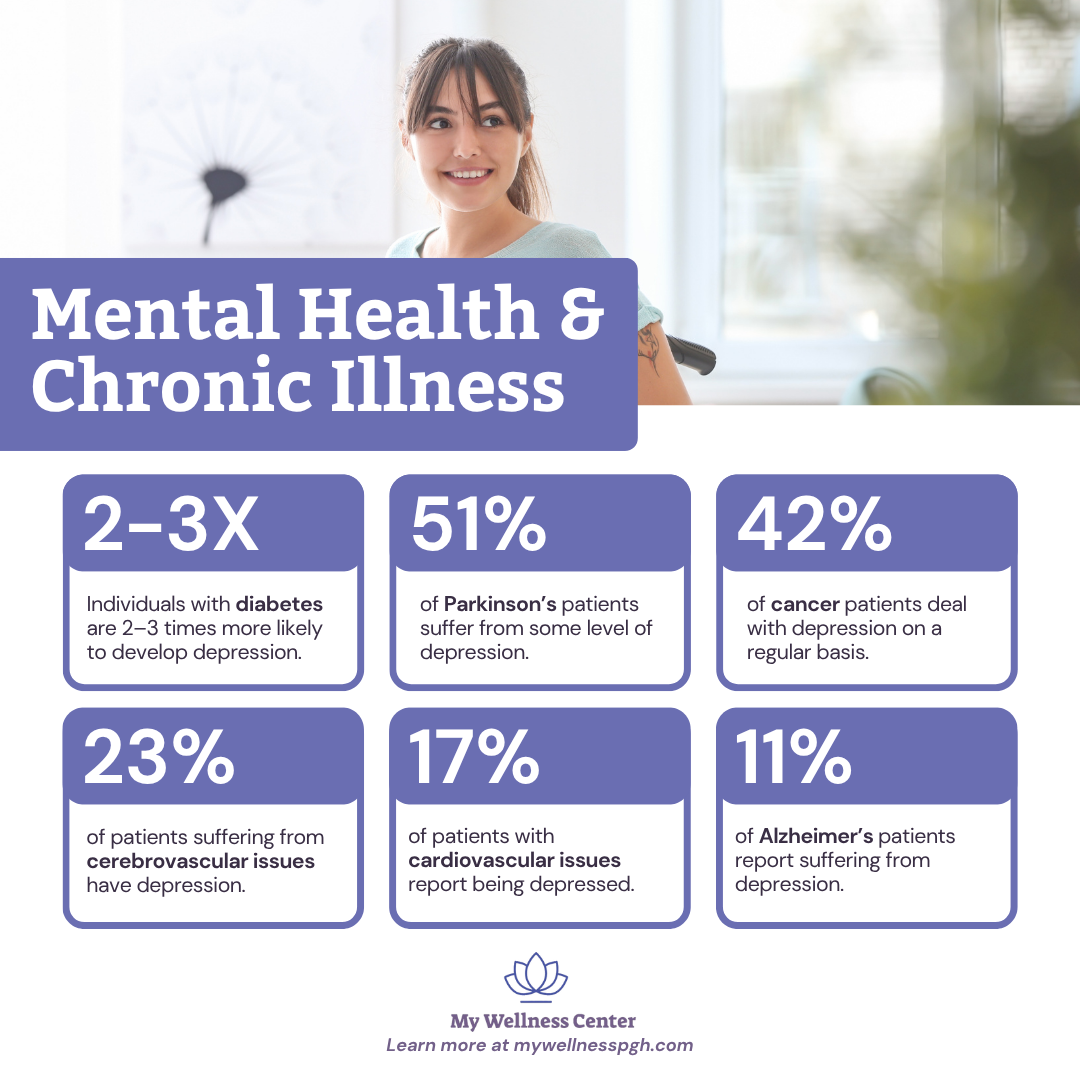
Statistics On Mental Health & Chronic Illness
Unfortunately, individuals with chronic disease are more likely to suffer from depression and other mental health issues. Keep in mind: Among the general population, about 4%–8% of people suffer from depression.
Here’s what some of the research shows:
- Diabetes – Individuals with diabetes are 2–3 times more likely to develop depression than people without diabetes. (Source: CDC)
- Parkinson’s – 51% of patients have depression (Source: Johns Hopkins)
- Cancer – 42% of patients have depression
- Cerebrovascular Issues– 23% of patients have depression
- Cardiovascular Issues – 17% of patients have depression
- Alzheimer’s – 11% of patients have depression
The combination of mental health issues and chronic illness can lead to a vicious cycle: Poor mental health leads to poor self-care, which exacerbates pre-existing conditions.
Research has also shown that individuals with chronic diseases are at an increased suicide risk. According to a study in the American Journal of Preventive Medicine, individuals may be at a higher risk if they suffer from:
- asthma
- back pain
- brain injury
- cancer
- congestive heart failure
- diabetes
- epilepsy
- HIV/AIDS
- heart disease
- high blood pressure
- migraine
- Parkinson’s
Related Reading: Is Suicidal Ideation Normal? Understanding the Difference Between Passive and Active Suicidal Ideation
Complications With Chronic Disease & Mental Illness
Everything is more difficult with chronic disease. For me, I’ve found crutches may provide limited relief for my knee, but they also make everything more challenging—both physically and mentally.
To properly use my crutches, I have to plan out tasks that used to be simple parts of my day:
- How will I get the soup out of the microwave without spilling it?
- How will I get from the car to my front door while carrying my belongings?
- How will I carry the laundry basket from the dryer to my bedroom?
It’s exhausting—and I’m not even dealing with a life-threatening illness!
Here’s why chronic disease can be so damaging to mental health:
1. Interference with Self‑Care
When a condition limits mobility, energy, or routine functions, simple self‑care tasks become monumental. For example, you may find it harder to maintain your exercise routine, eat nutritiously, or keep consistent sleep patterns.
The National Institute of Mental Health notes that people with chronic diseases are at higher risk for depression in part because of new challenges that interfere with healthy choices—like getting to the gym or cooking a nutritious meal.
What’s more, the constant demand of monitoring symptoms, managing medications, and attending appointments can leave little mental space for nurturing oneself.
2. Mental Exhaustion & Cognitive Load
Disease management frequently involves continuous decision‑making. For example, you might constantly ask yourself:
- What can I do today?
- How much energy do I have?
- Should I push through or rest?
The endless barrage is exhausting, especially since even mundane tasks require extra forethought. This kind of mental load leads to physical, mental, and emotional drain.
Research around chronic physical illness points out that living with long‑term conditions often forces people to adjust their aspirations, lifestyles, and employment, and these major adjustments can trigger grief reactions and persistent distress.
Related Reading: Therapy for Grief and Loss
3. Social Withdrawal & Isolation
Chronic illness can limit social engagement in several ways:
- You might skip outings because fatigue is overwhelming.
- You might worry about not being able to keep up with friends and family.
- You might feel embarrassed about needing assistance or accommodations.
Over time, fewer social connections can lead to loneliness and increased vulnerability to anxiety and depression.
The Mental Health Foundation states that people with long‑term physical conditions are “more than twice as likely to develop mental ill‑health” partly because of such cumulative isolation effects.
4. Loss of Identity and Role Shifts
Chronic illness often alters what you can do, thereby shifting how you see yourself and how others see you.
If you were once an active person, a caregiver, or a high‑performing employee, adjusting to new limits can trigger existential questions: Who am I now? What value do I bring?
These role disruptions can feed frustration, resentment, and sadness.
5. Vicious Cycle of Declining Physical And Mental Health
Chronic health issues lead to persistent mental health challenges, and these challenges worsen physical health—leading to a potential downward spiral.
For instance, one study found that individuals with depression and anxiety had higher rates of accumulating chronic conditions.
Untreated mental health struggles can hamper self‑care, medication adherence, exercise, and diet, which in turn worsen the physical disease and generate more emotional strain.
6. Financial Stress & Resource Burdens
Though not always front of mind, chronic illness often creates new financial burdens, such as:
- medical bills
- special medical equipment
- unplanned time off work
- time to travel to specialists
The stress of navigating insurance, fitting treatments into your budget, and fear of future costs can contribute to anxiety and depression.
Healthcare analyses show that when mental health disorders co‑occur with chronic disease, the cost of care rises significantly—and worse outcomes follow.
In fact, data from the CDC shows the cost of caring for people with chronic disease and mental health issues accounts for 90% of the country’s healthcare expenses.
7. Feelings of Helplessness & Uncertainty
When pain lingers, mobility declines, or treatments plateau, many feel powerless or stuck.
Constantly running through questions like “Will I experience another flare up?” or “Will I be able to walk tomorrow?” is a terrible source of ongoing distress.
Mental Health Therapy For Chronic Disease
If you’re suffering from a chronic illness, treating the physical symptoms isn’t enough. Mental health care should become an equal focal point in your journey.
Your therapist may determine that some of the following treatment strategies are appropriate for you:
1. Acceptance and Commitment Therapy (ACT)
ACT helps you face what cannot (yet) be changed, accept the reality of illness or limitations, and commit to actions aligned with your values. ACT offers a way to say, “Yes, I’m in pain,” and then ask, “How do I still live a meaningful life despite this?”
Research in chronic conditions suggests that these value‑driven interventions can reduce emotional distress and improve functioning.
2. Cognitive Defusion
When chronic illness generates unhelpful thoughts—“My body has betrayed me,” “I’ll never be normal again,” “Everyone’s judging me”—the risk for depression or anxiety escalates. Cognitive Behavioral Therapy (CBT) techniques and defusion strategies help by redirecting thoughts.
For instance: instead of “I feel worthless because I can’t carry laundry,” defusion helps you notice the thought and then observe it rather than fully believing it.
Studies of psychosocial interventions with adults newly diagnosed with chronic conditions found that CBT support had meaningful benefits, especially when treatment helped patients find additional resources.
3. EMDR for Chronic Illness‑Related Trauma
Though EMDR (Eye Movement Desensitization and Reprocessing) is often associated with PTSD, emerging research indicates it can be helpful when chronic disease intersects with trauma.
- reducing pain
- overcoming sleep difficulties
- easing depression
- reducing traumatic stress symptoms
Related Reading: PTSD vs. PTSS: Differences, Symptoms, and Treatment
4. Integrated Care: Blending Physical & Mental Health
Therapeutic success with chronic disease often comes from integrated care. One study found that embedding mental‑health services in chronic disease management helped patients improve both physical and psychological outcomes.
For example, your therapist might coordinate with your orthopedic surgeon, physiotherapist, or pain clinic so you’re not just treating “knee pain” and “mood” separately.
In addition, addressing lifestyle factors such as sleep, movement, and nutrition in therapy counts as mental‑health work when the body is your constant challenge.
5. Behavioral Activation & Values‑Consistent Living
Pain and physical limitations often pull you away from previously meaningful activities you used to enjoy—like hobbies, social roles, and exercise.
Therapy can help you re‑engage in modified ways. A couple of examples:
- chair yoga instead of full aerobic exercise
- adaptive social events instead of high‑mobility outings
Modifying the activities you love protects your mental health and reinforces a sense of identity beyond your illness.
6. Mindfulness & Somatic Awareness
Chronic illness often entails somatic signals (pain, stiffness, fatigue) that dominate your awareness.
Mindfulness helps you:
- notice sensations without spiraling
- develop tolerance for discomfort
- shift your focus to moment‑by‑moment experiences rather than a “ruined future”
7. Peer Support and Psychoeducation
Therapy is enriched when combined with peer groups or education about chronic illness. Understanding why feelings of helplessness, identity loss or fatigue are normal for those with chronic illness can reduce self‑blame.
8. Relapse Prevention & Resilience Building
Chronic illness often means good days and bad days. Therapy helps you anticipate “flare days,” build coping plans, reconnect with values even when pain spikes, and maintain hope.
Back to my knee pain: If I’m experiencing an especially painful day, I might pick a value-driven action that boosts my boost. I could call a close friend, stretch in my office chair, or journal about a positive memory.
Pittsburgh Mental Therapy for Chronic Pain & Illness
Don’t battle chronic pain alone. Our Pittsburgh therapists are here to help you navigate pain through the latest mental health therapy techniques, offering resources and strategies for living a happier, healthier life.
Contact us to get started.

